Rev Med UAS
Vol. 13: No. 4. Octubre-Diciembre 2023
ISSN 2007-8013
Crystell Guadalupe Guzmán-Priego1, Sergio Quiroz-Gómez1*, Karla del Socorro Celorio-Méndez1, Guadalupe del Carmen Baeza-Flores2, Obed Calles-Jiménez1, Nadia Guadalupe López-Jiménez1
*Autor de correspondencia: Sergio Quiroz Gómez Sergio
quiroz@ujat.mx Universidad Juárez Autónoma de Tabasco, División Académica de Ciencias de la Salud.
Gregorio Méndez 2838-A Col. Tamulté. Tel. (993) 3581500 Ext. 6300, 3581581 ó 354 02 92 CP. 86100.
Villahermosa, Tabasco, México.
DOI http://dx.doi.org/10.28960/revmeduas.2007-8013.v13.n4.005
Texto Completo PDFRecibido 05 de septiembre 2023, aceptado 22 de noviembre 2023
RESUMEN
Objetivo: Calcular el costo de la polifarmacia en pacientes ancianos con DM2. --- Metodología: se seleccionaron 104 registros clínicos de los núcleos básicos de un Hospital General de Tabasco, de pacientes adultos mayores con DM2. Se registró el consumo de fármacos y las patologías presentes; se estimaron el costo de los medicamentos y la demanda de servicios de salud. --- Resultados: Se encontró que el 50% de los pacientes sufren de hipertensión arterial además de DM2; 69.23% usan 6 medicamentos; 28.85% de los pacientes acudieron a 6 consultas; la percepción anual del personal de servicios de salud fue de $3,652,140.2 MXN para médicos, $2,250,853 MXN para enfermería, y $290,205.60 MXN para el personal de la farmacia. --- Conclusión: Promover la atención primaria es esencial para reducir la incidencia de enfermedades crónico-degenerativas que, junto con el envejecimiento, conducen a la polifarmacia y a un mayor costo de atención por paciente.
Palabras clave: polifarmacia, personas adultas mayores, diabetes mellitus, costo de fármacos, costo de la atención médica
ABSTRACT
Objective: Calculate the cost of polypharmacy in elderly patients with DM2. --- Method: 104 clinical records of the basic nuclei of a General Hospital in Tabasco of elderly patients with DM2 were selected. The consumption of drugs and present pathologies were recorded; the cost of drugs and the demand for health services were estimated. --- Results: It was found that 50% of the patients suffer from arterial hypertension in addition to DM2; 69.23% use 6 drugs; 28.85% of the patients came to 6 consultations; the annual perception of health services personnel was $3,652,140.2 MXN for doctors, $2,250,853 MXN for nursing, and $290,205.60 MXN for pharmacy personnel. --- Conclusion: Promoting primary care is essential to reduce the incidence of chronic-degenerative diseases that, together with aging, lead to polypharmacy and a higher cost of care per patient.
Keywords: polypharmacy, aged, Diabetes Mellitus, Drug Costs, Health Care Costs
Introduction
The number of older adults has increased considerably in the 21st century.1,2 According to UN data, between 2015 and 2050, the proportion of the world population over 60 years of age will go from 12% to 22%.2 In Mexico, 12.01% of the population is older than 60 years.3
Longer life expectancy increases morbidity and deterioration of health, therefore, increases the demand for care and the prescription of drugs.1,4 In Mexico it is estimated that the prevalence of polypharmacy in older adults is 55-65%.5 The population transition increases the suffering of chronic non-communicable diseases, the use of drugs, consequently, the prevalence of polypharmacy increases, a greater risk of prescription errors, adverse effects, drug interactions, among others.6
According to the WHO, diabetes mellitus is among the leading causes of mortality worldwide.7 In 2021, deaths from diabetes in Mexico ranked third with 15.87% of which 51.8% correspond to the group of older adults.8
This population group is vulnerable to the complications of the disease due to the physiological process of aging that increases the infiltration of fat in the tissues, greater risk of being overweight, malnutrition and less physical activity, in addition to the use of concomitant medications.9,10
The prevalence of diabetes in Mexico is 10.6% based on ENSANUT 2021; which also reports that 25.5% correspond to older adults.11 In the case of the state of Tabasco, the SVEHDMT2 Report places it as the state with the highest number of hospital admissions of patients diagnosed with diabetes.12 As a special case, the Tenosique hospital is considered, in order to categorize the economic expense for medical care.
The economic burden represented by the treatment of diabetes and its complications is very high. In Mexico, the costs are covered by patients or relatives and by health institutions.13 In a profitability analysis of the multidisciplinary health care model for patients with type 2 diabetes carried out in the public sector in Mexico, it was estimated that the average costs per patient in an average of 10 years reach $41,349.64 MN (2,188.97 USD) in a multidisciplinary care model and $43,494.41 MN (2,302.51 USD) in a conventional care model.14
Costs may vary if the patient is on monotherapy, combination therapy, or polypharmacy.15 It is important to recognize that this problem generates a relevant financial demand for the population and health services.16-17 For this reason, society must be made aware to correct the modifiable factors that are part of diabetes and, in this way, reduce its prevalence and costs.
Materials and methods
Descriptive quantitative study whose study population corresponds to 104 clinical records from a General Hospital in Tenosique, Tabasco. Inclusion-exclusion criteria were used based on the files that complied with NOM-004-SSA201218, which were of elderly patients diagnosed with type 2 diabetes and polypharmacy.
For data collection, a clinical record evaluation sheet divided into three domains was used. The first domain catalogs the sociodemographic data of the patients. The second domain consists of 12 items that record the patient's admission, initial management, polypharmacy, and comorbidities. The third domain consists of a table of drugs grouped according to the most frequent chronic pathologies in the elderly where the total number of drugs received in a year, the unit price and the subtotal of each section are recorded.
The drugs placed on the evaluation sheet are registered in CAUSES 2019 (Universal Catalog of Health Services). The prices of the drugs were taken from the acquisition list of drugs associated with CAUSES, published in the Official Gazette of the Federation on July 7, 2016.
The total annual economic income of each of the health workers who participated in the study (doctors, nurses, and pharmacy managers) was considered.
The cost evaluation in polypharmacy was evaluated based on three areas. Area 1 was the medical service identified by the number of visits attended per year by the unit price. Area 2 was the cost of drugs that was evaluated by annual consumption, as well as by unit cost. Area 3 was the cost of the pharmacy service that was determined by the number of visits to this service times the unit cost.
Results
The sociodemographic profile of the population studied, with a total of 104 patients, shows that the largest number of patients was in the range of 60-64 years with a result of 51% (n=53); the female gender predominated with 75-96% (n=79); illiterate or incomplete primary education with 38.46% (n=40); profession was housework with 72.12% (n=75); Marital status was widowed with 41.35% (n=41).
Of the total study population, 65.38% (n=68) of the patients presented the diabetes symptomatology record together with the figures of the laboratory analysis results that established the diagnosis in the admission note, and in 34.62 % (n=36) only a record of the symptoms was found, without laboratory results. The diagnosis of type 2 diabetes was determined in 88.46% (n=92) by means of the fasting plasma glucose test and 11.54% (n=12) was made by means of the postprandial plasma glucose test.
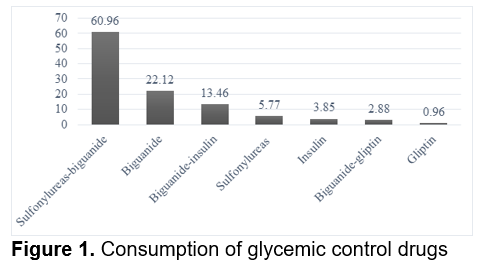
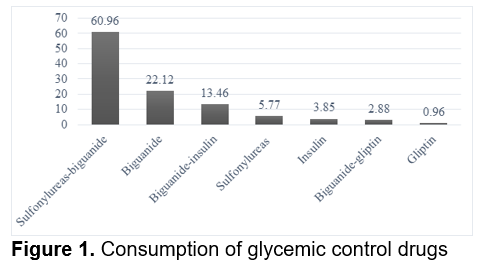
Of the patients who received pharmacological management, 54.81% (n=53) presented symptomatic hyperglycemia, while 45.19% (n=51) presented asymptomatic hyperglycemia. In relation to the use of hypoglycemic drugs, sulfonylureas-biguanides correspond to the highest percentage, with 60.96% (n=58); followed by the biguanides, with 22.12% (n=21); then the combination of biguanides-insulin, with 13.46% (n=13); sulfonylureas, with 5.77% (n=5); insulin, with 3.85% (n=4); the combination of biguanide-gliptin with 2.88% (n=2), and the gliptins, with 0.96% (n=1). (Figure. 1).
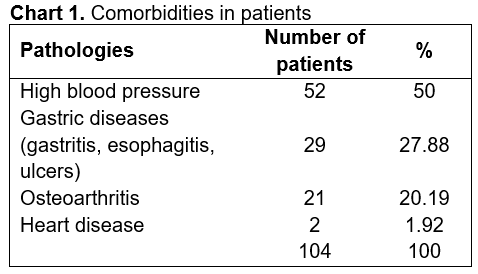
It was found that 81.73% (n=78) of the patients presented a pathology associated with diabetes; followed by 16.35% (n=16) of the patients who presented two, and only 1.92% (n=10) presented three. The most frequent pathology associated with the study population corresponds to arterial hypertension, with 50% of the total (n=52); followed by gastric diseases (gastritis, esophagitis, ulcers), with 27.88% (n=29); the presence of osteoarthritis, with 20.19% (n=21) and finally heart disease, with 1.92% (n=2) (Chart 1).
In relation to the number of drugs used by patients, the use of 6 drugs was found first, with 69.23% (n=72); followed by the use of 4 drugs, with 18.27% (n=19); then the use of 5 drugs, with 9.62% (n=10); the use of 7 drugs, with 1.92% (n=2), and finally the use of 10 drugs, with 0.9% (n=1). Of the total study population, 49.04% (n=49) of the patients used antihypertensive drugs; 27.88% (n=30) used gastric mucosa protectors; 21.15% (n=23) used NSAIDs and steroids, and finally, 1.92% (n=2) used cardiovascular drugs.
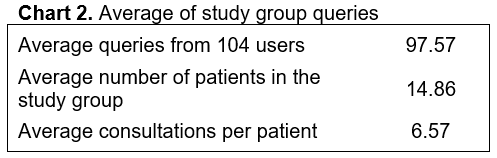
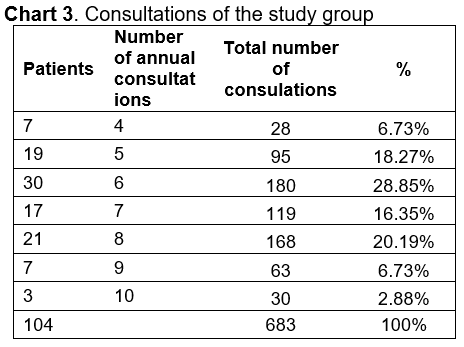
According to the number of consultations granted per patient registered in the files, the predominance of 6 consultations is contemplated, with 28.85% (n=30); followed by 8 consultations, with 20.19% (n=21); then with 5 consultations, with 18.27% (n=19); 7 consultations with 16.35% (n=17); 4 and 9 consultations with 6.73% (n=7) both, and finally with 10 consultations, 2.88% (n=3) (Chart 2).
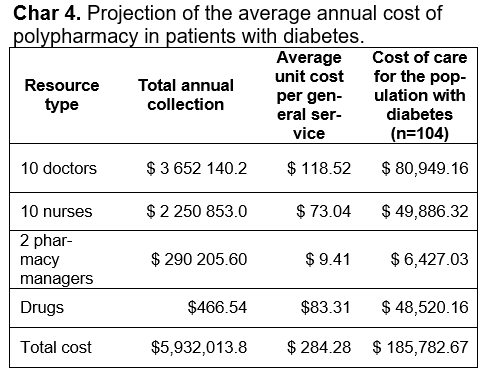
Based on the basic nuclei studied, the medical personnel (total of 10 people, one for each nucleus) had an annual perception of $3,652,140.2 MXN; the nursing staff (in a total of 10 people, one for each nucleus) had an annual perception of $2,250,853 MXN, and for the personnel in charge of the pharmacy (two people, one for each shift) had an annual perception of $ 290,205.60 MXN (Chart 3 and 4).
Discussion
The analysis of polypharmacy in the elderly with type 2 diabetes is a public health problem that is increasing due to the existing demographic transition both in the Mexican population and in most countries18.
Regarding the sociodemographic profile of the study patients, the elderly person was 60 years of age or older; with a predominance of female patients between the ages of 60 and 64, being consistent with the results of Pérez Lozano et al, where the predominance was also female patients with an age range of 61 to 70 years.
Regarding the daily consumption of drugs, it was determined that 69.23% of patients use 6 drugs. Pérez Lozano et al in their article mention an average of 52% of patients who used 2 drugs and only 16% had a polypharmacy treatment, being a higher result in this study.
In the use of hypoglycemic drugs, it was obtained that 60% of the patients had a combined treatment of sulfonylureas-biguanides, consistent with the results of the author Pérez Lozano et al, where the sulfonylurea-treatment is presented as a predominance in dual therapies. biguanides.
In section two of the study, it is stated that 65.38% of the records presented a record of the symptoms and confirmatory analysis of the diagnosis of Type 2 Diabetes Mellitus, which indicates that most of the doctors of the General Hospital of Tenosique determine the diagnosis of Diabetes Mellitus type 2. admission of the patient in accordance with the provisions of NOM-015-SSA2-2010. Thus, 88% of the patients were diagnosed with fasting plasma glucose and 11.54% with postprandial plasma glucose.
Referencias