Rev Med UAS
Vol. 12: No. 2. Abril-Junio 2022
ISSN 2007-8013
Oscar Gerardo Figueroa-Salcido1,2, MSc; Feliznando Isidro Cárdenas-Torres2, PhD; Francisco Cabrera-Chávez2, PhD; Jhonatan González-Santamaría2,3, PhD; Jesús Gilberto Arámburo-Gálvez1,2, MSc; Verónica López-Teros1, PhD; Humberto Astiazaran-García4, PhD; Noé Ontiveros5* , PhD.
* Corresponding Author: Noé Ontiveros Apodaca.
Lázaro Cárdenas del Río No.100, Francisco Villa, Navojoa, 85880 Navojoa
Email address: noe.ontiveros@unison.mx
DOI http://dx.doi.org/10.28960/revmeduas.2007-8013.v12.n2.004
Texto Completo PDFRecibido 15 de febrero 2022, aceptado 05 de marzo 2022
RESUMEN
Objetivos: Estimar la prevalencia por auto-reporte de trastornos relacionados al consumo de gluten (TRG) y adherencia a una dieta libre de gluten (DLG) en una población colombiana y caracterizar a aquellos que siguen una DLG, evitan o incluyen el gluten en la dieta. --- Material y Métodos: Se realizó una encuesta en línea utilizando un cuestionario validado y adaptado culturalmente. --- Resultados: Considerando 850 respuestas válidas (52.2%), las tasas de prevalencia fueron/IC 95%: reacciones adversas recurrentes al trigo/gluten (RAR-T/G) 9.29%/7.52-11.43, alergia al trigo 0.47%/0,18-1.20, sensibilidad al gluten no celíaca (NCGS) 2,35%/1,52-3,60 y adherencia a la DLG 6.94%/5.41-8,85. No se encontraron casos de enfermedad celíaca (EC). Los diagnósticos de TRG se basaron en los síntomas (85.71%). Entre 79 casos de RAR-W/G o 100 de síndrome de intestino irritable (SII), solo 8/79 y 5/100 tenían diagnóstico médico de NCGS, pero pruebas celíacas fueron informadas por solo un caso. La DLG fue instruida en algunos casos por un profesional de la salud (49.15%). El control de peso (74.42%) y la percepción de que una DLG promueve la salud (46.51%) fueron las motivaciones para apegarse a la DLG. --- Conclusiones: Existe un subdiagnóstico potencial de EC en Colombia, incluso, la mayoría de los que tienen diagnóstico médico de SII y RAR-T/G no han sido evaluados para EC. Similarmente, los diagnósticos médicos de NCGS raramente incluyen pruebas celíacas, lo que genera dudas sobre el diagnóstico y el seguimiento del paciente. Finalmente, se debe informar a la población colombiana sobre los riesgos/beneficios de seguir una DLG sin asesoría profesional.
Palabras Clave: Gluten, NCGS, Enfermedad Celíaca.
ABSTRACT
Objectives: To estimate the self-reported prevalence of gluten-related disorders (GRDs) and adherence to a gluten-free diet (GFD) in a Colombian population and to obtain the characteristics of GFD followers, gluten avoiders, and non-avoiders. --- Material and Methods: A survey was conducted using a culturally adapted and validated questionnaire. --- Results: Considering 850 valid responses (52.12%), the prevalence rates were/95% CI: Recurrent adverse reactions to wheat/gluten (RAR-W/G) 9.29%/7.52-11.43, wheat allergy 0.47%/0.18-1.20, non-celiac gluten sensitivity (NCGS) 2.35%/1.52-3.60, and GFD adherence 6.94%/5.41-8.85. No celiac disease (CD) cases were found. Most GRDs diagnoses were symptom-based (85.71%). Among 79 RAR-W/G or 100 irritable bowel syndrome (IBS) cases, only 8/79 and 5/100 had a physician diagnosis of NCGS, but celiac tests were informed by only one case. Health professionals were instructing the GFD in 49.15% of the GFD cases. GFD adherence motivations included weight control (74.42%) and the perception that a GFD promotes health (46.51%). --- Conclusions: There is a potential subdiagnosis of CD in Colombia, and even the majority of those with a physician diagnosis of IBS and RAR-W/G do not have undergone CD assessment. Similarly, physician-diagnosed NCGS cases rarely undergo celiac tests, raising questions about the optimal patient’s diagnosis and follow-up. Finally, the Colombian population should be informed about the risks/benefits of following a GFD without professional counseling.
Keywords: Gluten, NCGS, Celiac Disease.
Introduction
Gluten-related disorders (GRDs) such as celiac disease (CD), wheat allergy (WA), and non-celiac gluten sensitivity (NCGS) can be triggered in susceptible individuals after wheat/gluten intake. In Colombia, information about the epidemiology of GRDs and adherence to a GFD is emerging. A study carried out five years ago concluded that among 1,207 adult Colombians surveyed face-to-face, none declared a CD diagnosis, although the prevalence of recurrent symptomatic adverse reactions to oral wheat/gluten (RAR-W/G) was high (5.9%)1. More recently, others concluded that the serogenetic prevalence of CD in Colombia is 1.32%, which is as high as in other countries2. These facts highlight not only the lack of awareness of CD but also a potential misdiagnosis of other GRDs. Additionally, it should be noted that CD serology is cost-effective and recommended in patients with irritable bowel syndrome (IBS) among which the prevalence of CD is higher than 1%3. In this context, the self-reported physician-diagnosed prevalence of IBS in Colombian adults is 8.9%, but the characteristics of the IBS cases with regard to RAR-W/G or the diagnosis of GRDs have not been addressed in detail1. Additionally, current evidence highlights that the prevalence of adherence to a GFD is high in Colombia and that most subjects following the diet have neither received a diagnosis of GRDs nor triggered adverse reactions after consumption of wheat/gluten. However, the motivations for following a GFD and who instructs the diet are issues that have not been addressed in the Colombian population. Thus, the aim of the present study was to estimate by self-report the prevalence of GRDs and adherence to a GFD in a Colombian population and to obtain the characteristics of those with RAR-W/G following a GFD or doing their best or not to avoid wheat/gluten from their diets.
Material and Methods
Questionnaire, Data Collection, and Definitions
A validated questionnaire was adapted to obtain information about who established the diagnosis of GRDs and the diagnostic workup, the motivations for following a GFD and who instructs the diet, and the reasons for gluten-free dietary non-compliance in GRDs cases4. The web-based survey was conducted as follows: A digital version of the questionnaire was developed using the SurveyMonkey digital platform (San Mateo, CA, USA). The hyperlinks generated were sent via text messages to the adult population from Pereira, Colombia. Each participant was able to take the survey only once, and no reward was offered for taking it. The inclusion criteria were as follows: 1) Pereira, Colombia residents who agreed to participate in the study, 2) were 18 or older, and 3) were able to read and respond to the questionnaire on their own. Incomplete questionnaires were excluded from the analysis. Data were collected from the 06th of April to the 24th of June 2021.
The definitions used were described previously5. Briefly: recurrent adverse reactions to wheat/gluten (RAR-W/G); individuals that most of the time or always trigger symptoms after ingestion of wheat/gluten, self-reported gluten sensitivity (SR-GS); individuals that met the criteria for RAR-W/G and were on a GFD, or declared a medical diagnosis of CD, WA, or NCGS, SR-WA; individuals that met the criteria for RAR-W/G, were on a GFD, and declared symptoms characteristics of immediate-type food allergy (Most subjects fulfilling these criteria (93%) have IgE antibodies to the implicated food6), SR-NCGS; individuals that met the criteria for RAR-W/G, were on a GFD, did not meet the criteria for SR-WA, and did not declare a physician diagnosis of WA or CD, self-reported physician-diagnosed (SR-PD) CD, SR-PD WA, and SR-PD NCGS; individuals that declared that a physician diagnosed them.
Statistical analyses and ethical aspects
Data were analyzed using the statistical software GraphPad Prism Version 8.0 (GraphPad Software, San Diego, CA, USA). Categorical variables were expressed as percentages and/or total numbers. Associations were determined using a two-tailed Fisher’s exact test. A p value < 0.05 was considered statistically significant. Prevalence rates were estimated using the OpenEpi software version 3.03a and reported per 100 habitants (95% confidence intervals). The sample size was calculated considering the following parameters: 1) infinite population, 2) precision of 2%, 3) confidence interval of 95%, and 4) an expected prevalence of adverse reactions to oral wheat/gluten of 8.0%1. A sample size of at least 707 participants was considered representative. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Technological University of Pereira (CODIGO DE AVAL: 21- 050421; Apr 05, 2021).
Results
Participants’ characteristics
A total of 850 participants answered the questionnaire (valid response rate: 52.14%). The proportion of women was slightly higher than men (53.17% and 46.82%, respectively). Lactose intolerance (13.53%) and irritable bowel syndrome (IBS) (11.76%) were the most common physician-diagnosed conditions followed by non-food allergy (6.12%) and psychiatric disease (2.12%).
Prevalence rates
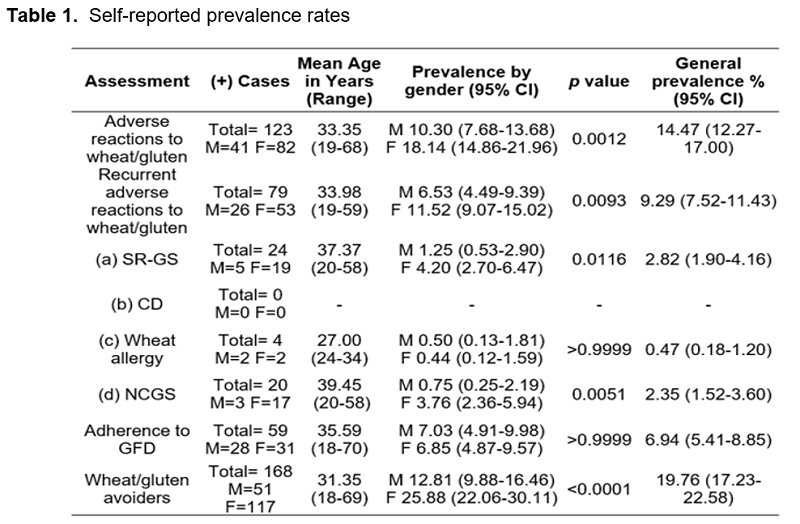
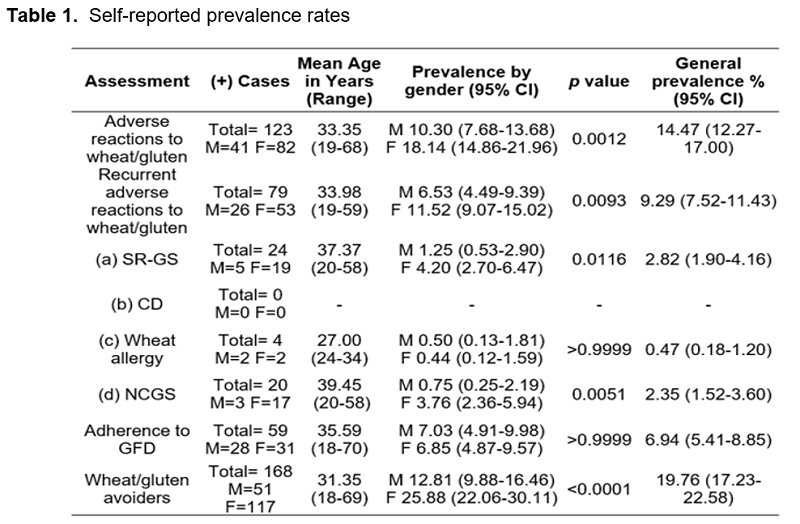
The estimated prevalence rates are shown in Table 1. No CD diagnoses were found. The prevalence rates of SR-GS, WA, and NCGS were 2.82% (95% CI; 1.90-4.16), 0.47% (95% CI; 0.18-1.20), and 2.35% (95% CI; 1.52-3.60), respectively (Table 2). More women than men declared adverse reactions to oral wheat/gluten (p < 0.0012) and met the criteria for RAR-W/G (p < 0.0093) (Table 1). Similarly, the prevalence rates of SR-GS and NCGS were higher in women than in men (p < 0.0116 and p < 0.0051, respectively) (Table 1). The prevalence of gluten avoiders was 2-fold higher in women than in men (p < 0.0001) (Table 1).
Self-reported diagnostic workup of GRDs
Twelve subjects met the criteria for SR-PD GRDs. Another case declared that a dietitian diagnosed him/her. General practitioners (n=6), gastroenterologists (n=5), homeopaths (n=3), or allergists (n=1) made the diagnoses, but only 1 case underwent celiac serology and 2 oral challenges. Two cases were diagnosed by more than one physician and 5 declared a physician diagnosis of IBS. Overall, 83.33% (10/12) or 76.92% (10/13) of the GRDs cases diagnosed by physicians (SR-PD GRDs) or health professionals were symptom-based diagnoses, respectively.
Characteristics of subjects following a GFD and gluten avoiders
A total of 59 subjects were following a GFD, but only 16 (27.11%) of them met the criteria for SR-GS. Overall, 50.0% (n=10/20) of the cases that met the criteria for NCGS (either self-reported or PD) also declared a physician diagnosis of IBS. Regarding those that were diagnosed by a physician (either WA or NCGS), only 4 out of 12 cases were following a GFD (33.33%).
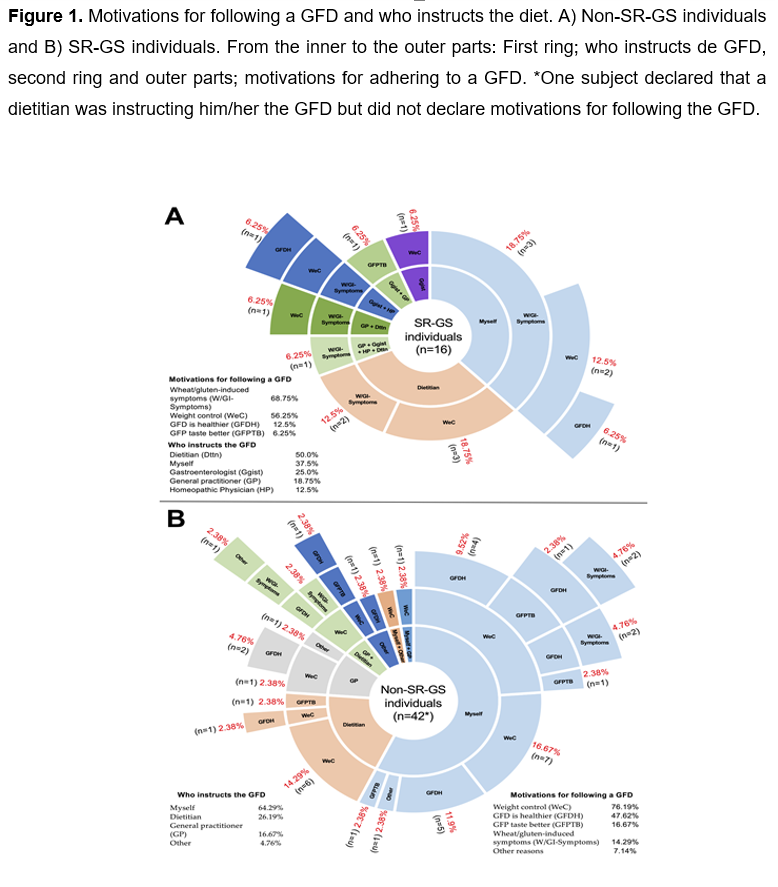
Figure 1 shows the motivations for following a GFD and the information about who instructs the diet. 37.50% of the individuals in the SR-GS group and 55.81% in the group of individuals that did not meet the criteria for SR-GS (non-SR-GS group) were following a GFD without gluten-free dietary counseling, respectively (p = 0.2516) (Figure 1A and 1B). Overall, 50.85% (n=30) of the participants on a GFD were following the diet without dietary counseling. The main motivations for following a GFD between the SR-GS and non-SR-GS groups were weight control (56.25% vs 76.19% (p = 0.1970)), the perception that a GFD is healthier (12.50% vs 47.62% (p = 0.0164)), and the oral wheat/gluten induced symptoms (68.75% vs 14.28% (p = 0.0001)) (Figure 1A and 1B). Statistical comparisons by gender were not significant (p > 0.05).
The reasons for gluten-free dietary non-compliance among those that met the criteria for SR-PD GRDs were the low availability (n=4/8) and the high cost of gluten-free products (n=3/8), and the mildness of the symptoms triggered after consumption of wheat/gluten (n=2/8). The characteristics of the gluten avoiders (n=40) (doing their best to avoid wheat/gluten from their diets) and wheat/gluten non-avoiders (n=23) who met the criteria for RAR-W/G are shown in Figure 2. For both groups -the wheat/gluten avoiders and non-avoiders with RAR-W/G- the reasons for not being on a GFD were the high cost and the low availability of gluten-free products, and the mildness of the symptoms triggered after consumption of wheat/gluten (Figure 2). Statistical comparisons of the reasons/motivations for not being on a GFD or for avoiding wheat/gluten from the diet by gender were not significant (p > 0.05). Furthermore, among the gluten avoiders and non-avoiders with RAR-W/G and a physician diagnosis of IBS (33.33% n=21/63) (Figure 2), three of them have a physician diagnosis of NCGS, but they did not undergo CD assessment. The others (n=18) neither met the criteria for WA nor had a CD diagnosis.
Taken together, among 79 RAR-W/G cases, 56 (70.88%) were either on a GFD (n=16) or doing their best for avoiding wheat/gluten from their diets (n=40) (Figures 1A and Figure 2, respectively), 4 met the criteria for WA, 28 had a physician diagnosis of IBS (non-WA cases), 8 had a physician diagnosis of NCGS (only 1 underwent celiac serology evaluations) (figures 1 and 2), and no one had a diagnosis of CD. In other context, among 100 physician diagnosed IBS cases, 12 were following a GFD (6 because of the symptoms triggered after ingestion of wheat/gluten), 29 were doing their best for avoiding wheat/gluten from their diets (16 met the criteria for RAR-W/G (Figure 2)), no one have diagnosis of CD, and 5 have physician diagnosis of NCGS (only 1 underwent celiac serology evaluations). Overall, 28 physician diagnosed IBS cases met the criteria for RAR-W/G (7 gluten-free followers, 16 gluten avoiders, 5 gluten non-avoiders).

Discussion
In the present study, a web-based survey was conducted in Colombia to estimate the self-reported prevalence of GRDs and adherence to a GFD. The questionnaire utilized was taken from a previous face-to-face survey carried out in Antioquia, Colombia1, but it was adapted to inform for the first time about the diagnostic workup of SR-PD GRDs cases and about the characteristics of those with RAR-W/G following or not a GFD. The current self-reported prevalence of WA in adult Colombian population (0.47%) is in line with most self-reported prevalence rates estimated in other Latin American countries (0.33-0.79%)4,5,7,8 and even in Colombia five years ago (0.74%)1. The prevalence rates of RAR-W/G and NCGS were 9.29% and 2.47%, which are 0.75 and 2.3 folds higher than the ones reported in a previous face-to-face survey (9.29% vs 5.30% and 2.47% vs 1.07%), respectively1. These results suggest that RAR-W/G could be increasing over the last years in Colombia and, consequently, more individuals believe that they are gluten sensitive. Increasing dietary wheat/gluten exposure is the main environmental factor to trigger GRDs in susceptible individuals, but the consumption of wheat has remained stable in Colombia over the last years9. In line with previous findings1, no CD cases were found in the present study highlighting a potential underdiagnosis of this condition, as the serogenetic prevalence of CD is around 1.32% in the Colombian population2. Overall, the results confirm that RAR-W/G are common in Colombia affecting more than 9.0% of the adult population and highlight the need to increase awareness about CD to prevent long-term complications such as nutritional deficiencies, osteoporosis, and lymphoma, among others10.
Most GRDs diagnoses made by health professionals were symptom-based ones (76.92%, n=10/13). The other GRDs diagnoses were based on celiac serology and gluten challenges (23.07%, n=3/13). Celiac serology and intestinal biopsies histology are the cornerstone for CD diagnosis, and gluten challenges are required for establishing the diagnosis of CD in patients already following a GFD11. Furthermore, gluten challenges can help to differentiate between NCGS and gluten-sensitive IBS cases as long as they are carried out according to the Salerno experts’ criteria, and both CD and WA have been properly ruled out, and the Rome IV criteria are applied3. With regards the gluten challenge, clear benefits while the patient is following a GFD and worsening upon gluten reintroduction has been proposed as a practical approach12. This differential diagnosis is relevant from a therapeutic point of view. While NCGS individuals will benefit from a wheat/gluten- and/or a FODMAPS-free diet, the therapeutic intervention for some IBS patients can include not only a GFD but also other restriction diets, and/or approved drugs for IBS (diarrhea-predominant, constipation-predominant, or mixed IBS)13,14. Notably, in the present study, 28 physician diagnosed IBS cases met the criteria for RAR-W/G, most of them were on a GFD or doing their best for avoiding wheat/gluten from their diets. In fact, 5 of these 28 IBS cases have physician diagnosis of NCGS, but only one of them underwent celiac tests. These results set a precedent to test for CD in the IBS Colombian population as the serogenetic prevalence of CD in this population is 1.32%2 and testing for CD in IBS cases is cost-effective and recommended if the CD prevalence is >1% 12. Additionally, the potential low number of celiac tests performed in individuals with RAR-W/G or with a physician diagnosis of NCGS can explain the absence of CD diagnoses by self-report in the Colombian population.
The GFD is the only available treatment for CD patients and, including wheat as a source of gluten, FODMAPS and other cereal grain components, is a therapeutic option for WA, NCGS, and some IBS patients. In the present study, the prevalence of adherence to a GFD was 6.94%, which is higher than the rates reported in some high-income countries (0.58-1.9%) 15 and similar to the prevalence reported in a Colombian population five years ago (5.9%)1. Certainly, the GFD is gaining popularity in part by the opinion of celebrities and sport individuals in social media about the self-perceived “benefits” for following the diet 16. In fact, online searches for gluten-free products, such as gluten-free oats, flours, cereals, and bread, have increased up to 700% in the last five years in Colombia, which highlights a growing interest for including this type of products into the diet (Google Trends, consulted October 10, 2021). Despite scientific evidence indicating that the GFD does not provide health benefits in the absence of GRDs, most participants on a GFD have not triggered adverse reactions after consumption of wheat/gluten and do not have a diagnosis of GRDs (72.88%). Their motivations for following the diet include weight control and the perception that a GFD promotes health; motivations widely recognized as misconceptions of the GFD 17. Most notably, up to 50.84% of those on a GFD have not had gluten-free dietary counseling by a trained health professional putting themselves at risk of a nutritional imbalance such as a reduced intake of folic acid, iron and calcium, and an increased intake of fats and sugar 17. Furthermore, an imbalanced GFD also increases the risk for developing metabolic syndrome, type 2 diabetes, and dyslipidemia18. Overall, the results suggest that actions are needed to inform the Colombian population about the scientifically sound risks and benefits of adhering to a GFD without the dietary counseling of a trained health professional.
Additionally, our findings show that most individuals with a physician diagnosis of GRDs (66.66%) or with RAR-W/G (79.74%) were not following a GFD. The main reasons for not being on a GFD were either the low availability or the high cost of gluten-free products, or both reasons (40%). Indeed, studies carried out in Latin America and elsewhere show that gluten-free products have low availability and are generally more expensive than their regular counterparts19,20. The implementation of government programs, such as tax reduction and prescription and subsidy, to reduce the economic burden of the GFD would benefit those formally diagnosed Colombians that require the GFD as a therapeutic option, and it could increase awareness among health professionals about the diagnostic workup of GRDs.
Conclusion
The results of the present study suggest that health professionals should adhere as much as possible to globally accepted guidelines for diagnosing GRDs due to RAR-W/G are common in the Colombian population, even in IBS patients, and there is a potentially high rate of NCGS diagnosis without the exclusion of CD. In this context, the absence of CD cases by self-report could be attributed to misdiagnoses of either NCGS or IBS. The results also show that there is a high rate of GFD adherence, but most people were on a GFD for keeping/reaching a healthy weight or for the ambiguous notion that a GFD is healthier than a regular one. Contrary, most people with RAR-W/G, with or without a diagnosis of a GRD, were not following a GFD because of the low availability and/or the high cost of gluten-free products. These data highlight that actions to inform the general population about the scientifically sound risks and benefits for following a GFD are desirable, as well as actions to reduce the economic burden for following a GFD as a therapeutic option.
Acknowledgements
The authors wish to thank CONACyT for the post-graduate fellowship given to O.G.F.-S and J.G.A.-G. The technical support by Carolina Villa, Natalia Mejía and Luisa Varona is also acknowledged.
Conflict of interest
Authors declare no conflict of interest.
Funding: This research received no external funding.
References