Rev Med UAS
Vol. 11: No. 4. Octubre-Diciembre 2021
ISSN 2007-8013
Eduardo Flores-Villalba1,2,*, Jose I Ortiz De Elguea-Lizarraga2, Victor Segura-Ibarra1,2, Elvia M Dominguez-Barragan2, Ana S Guerra-Cantu2, Jose A Diaz-Elizondo2, Marisa G. Frausto-Alejos2, Dixia Ramirez1
*Autor de correspondencia:Eduardo Flores-Villalba, MD, MSc
TEC de Monterrey, School of Medicine and Health Sciences
Ignacio Morones Prieto 3000 Pte. Col. Doctores Monterrey, NL., México, CP 64710
Email: eduardofloresvillalba@tec.mx
Phone: 52 (81) 88 88 03 10
DOI http://dx.doi.org/10.28960/revmeduas.2007-8013.v11.n4.003
Texto Completo PDFRecibido 01 de julio 2021, aceptado 28 de julio 2021
Abstract
Introduction: Surgical rotations of medical students are physically, emotionally, and intellectually demanding. Energy expenditure throughout a shift, lack of sleep and inadequate nutrition affect student’s performance. --- Objective: The aim of this study is to describe and analyze caloric intake and energy expenditure during a 24-hour shift in medical students during a clinical surgical rotation. --- Materials and Methods: Twenty-three medical students wore a smart armband during a 24-hour shift to register energy expenditure physical activity, along reports of meals and food intake. --- Results: Median energetic expenditure was of 3666 kcal/day while intake was of 1384 kcal/day, averaging a deficit of 2374 kcal. Students slept a median of 0 minutes and walked 9252 steps. Discussion and Conclusion: These parameters should be considered when designing clinical rotations to provide quality service to patients and ensure the well-being of students.
Key words: Caloric expenditure, medical students, Shifts, Clinical Internship
Resumen
Introducción: Las rotaciones clínicas de cirugía de los estudiantes de medicina son exigentes física, emocional e intelectualmente. El extraordinario gasto de energía que se tiene durante un turno quirúrgico, la falta de sueño y una nutrición inadecuada, afecta a los estudiantes de manera profesional y en su vida personal. --- Objetivo: Describir y analizar la ingesta calórica y el gasto energético durante un turno de 24 horas en estudiantes de medicina durante una rotación clínica de cirugía. --- Materiales y métodos: Veintitrés estudiantes de medicina usaron un brazalete inteligente durante un turno de 24 horas con el fin de obtener el gasto de energía, horas de sueño y actividad. Los estudiantes también reportaron cada comida e ingesta de alimentos durante su turno. --- Resultados: La mediana del gasto energético fue de3666 kcal/día y la mediana de ingesta fue de 1384 kcal/día, lo que llevó a un déficit calórico de 2374 kcal. Los estudiantes durmieron una mediana de 0 minutos y caminaron 9252 pasos. Discusión y conclusión:
Introduction
College students have a poor quality diet due to many factors: living away from home, scarce time dedicated to quality food preparation and other behavioral factors1. Medical students undergo excessive stress during their clinical rotations, which is another factor that greatly impacts their diets and eating habits. The typical 24-hour shift of medical students during a surgical clinical rotation consists of long periods that are physically, emotionally and intellectually demanding. Student’s tasks during their surgical shifts include wound cleaning, nasogastric tube placement, urinary catheter placement, medical history taking, and writing notes, between other activities. They are also frequently encountered with complex questions, which require continuous study and research during the shift. Most of the time, these shifts are so busy that medical students have little or no opportunity to sleep or eat, and when they do, it is usually poor-quality rest and meals2-4.
According to the Institute of Medicine, a regular diet should have 45-65% carbohydrates, 20-35% fat, and 10-35% protein5. When medical students have a chance to eat, they usually rely on fast food due to the short amount of time they can dedicate to this important aspect. Fast food is high in fats and carbohydrates but low in proteins and other micronutrients6.
On the other hand, sleep deprivation has been associated with decreased leptin levels and increased ghrelin levels which result in increased hunger7. Therefore, sleep deprivation can be directly linked with increased caloric intake and a positive nutritional balance.
Medical students are having a bad diet in terms of quantity and quality. Poor diets are associated with chronic health problems in the future like diabetes mellitus, hypertension, and even oncological problems8.
The aim of this study is to describe and analyze caloric intake and energy expenditure during a 24-hour shift in medical students during a clinical surgical rotation. We also measured the steps they took during the shift, total time of sleep, and the total time of activity.
Materials and Methods Prior informed consent, twenty-three medical students from TEC de Monterrey School of Medicine were enrolled from February to April 2015 during their surgical clinical rotation of 3 months at a public hospital in Monterrey, Mexico to participate in this survey.
Enrolled participants were weighted and measured the day before their shift. Students wore a SenseWear™/Armband (SWA) (BodyMedia, Inc. Pittsburgh, PA) during a 24-hour shift in order to attain energy expenditure, hours of sleep, and activity. Even though students usually stayed at the hospital for 32 hours, only the first 24 hours were analyzed from 7:00 am to the next day. Energy expenditure, sleep hours, and activity was estimated from the SWA proprietary equations developed by the manufacturer. Students sent pictures from every meal and food intake in real time via cell phone to our team. Portions from each meal were calculated according to Mexican National System of Food Equivalents (Sistema Nacional de Alimentos Equivalentes) (8). Most of the food intake (approximately 80%) was wrapped or canned food, so calorie intake was obtained from the label.Results
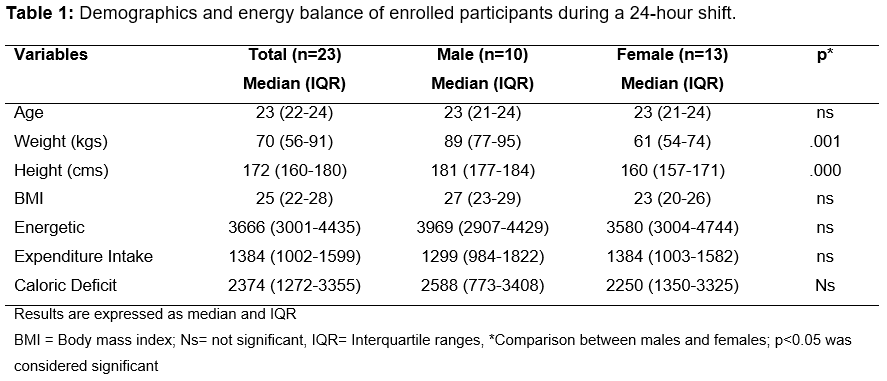
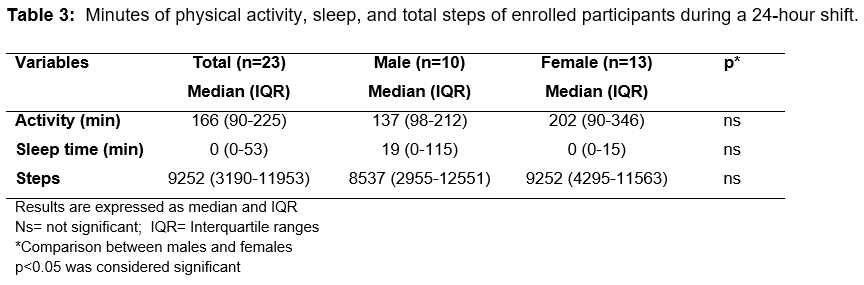
We analyzed 23 medical students, 10 (43.47%) males and 13 (56.52%) females. All of which concluded the study. The median height and weight was 171 cm and 71 kg. Median body mass index (BMI) was 25 kg/m2. We found a significant difference in weight (p<.001) and height (p<.000) between males and females. The median energetic expenditure was 3666 kcal/day and the median intake was of 1384 kcal/day, leading to a caloric deficit of 2374 kcal. (Table 1).
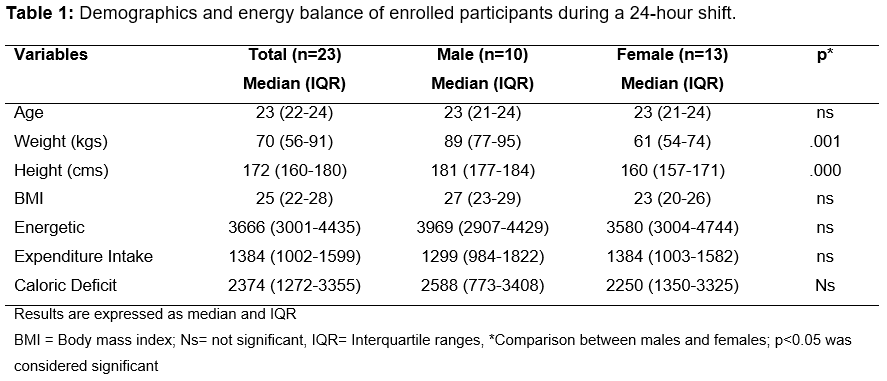
The medical students in our group had a median intake of 46% of carbohydrates, 38% of fat, and 16% of protein. We found that female students had a lower intake of proteins than male students with a significant (p<.049) difference (Table 2).
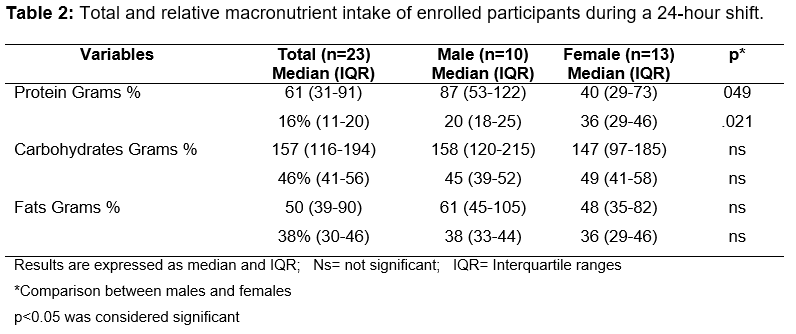
Medical students walked a median of 9252 steps during the 24-hour shift, which is equivalent to 166 minutes of continuous activity and they slept a median of 0 cero minutes (IQR 0-53) minutes in 24 hours with. (Table 3).
Discussion
Evidence suggests that college students have a poor-quality diet. Based on a diet quality index, it has been described that 77% of students need to improve their diet and that 21% had a very poor quality diet9. Poor quality diet in college has been associated to similar dietetic behaviors in adulthood, which represents a major risk factor for chronic degenerative diseases and even oncologic diseases, as mentioned previously 10.
According to the Dietary Guidelines for Americans 2010, college students should receive from 1800 to 2400 Kcal per day for women and from 2400 to 3000 Kcal for men11. In our study we found an average consumption of 1,458.45 kcal/day for males and 1350.18 kcal/day for females, approximately 1000 kcal/day less than previous reports. Moreover, our students met the definition of a hypo caloric diet even in a sedentary group.
In our study we measured the quantity of kcal consumed per day along with the energy expenditure, sleep time and activity during a 24-hour shift, enabling the calculation of a nutritional balance.
We found that in average, medical students had an energy expenditure of 3,833.83 kcal/day, resulting in an average negative balance of 2,436.57 kcal/day, which is twice the amount of calories an average 140 pounds person should spend. Surprisingly, one of our medical students had an energy expenditure of 6,833 kcal/day, which is in the realm of high performance athletes during intense training which have an energy expenditure from 4,200 to 7000 kcal 11.
Participants walked an average of 8,712 steps, the corresponding to walking approximately 4 kilometers and the equivalent to an average of 185 minutes of registered continuous activity.
Students at our program as well as most in many countries, run under an 80-hour per week program with 24-hour shifts every second day. During weekdays, they stay at the hospital for 8 more hours after their shift with a total of 32 hours average, and the day before their shift they work for 8 to 10 hours during daytime. Weekend shifts last 24 hours as well but they do not stay afterwards and if they are not on call, they do not attend clinical duties. According to our data, this means that at least 2 to 3 days a week, a medical student will spend twice the energy they consume. Wishnofksy´s rule states that 3,500 kcal are equivalent to 1 pound of weight mass 12. Using this rule, we can estimate that our students loose in average two pounds per week during their surgery clinical rotation.
As mentioned before, the problem is not entirely the caloric deficit that medical students are currently having. Even a normal caloric diet or a hyper caloric diet might lead to nutritional deficit due to the bad quality of the food ingested. Food with a large percentage of fat will supply the calories necessary but not all the nutriments and therefore will also lead to health problems at a long term. As mentioned previously, a regular diet for people from 19 to 30 years old should be divided in 45-65% carbohydrates, 20-35% fat, and 10-35% protein (5). Therefore, our group had a slightly high percentage of fat and a normal distribution of carbohydrates and proteins in their shifts with the inconvenience that 80% of food was wrapped or canned.
It is very important to state that nutritional deficiency is associated with many health problems. Micronutrient deficiency is associated with bad functioning of the immune system, predisposing to infectious diseases, which are currently encountered by medical students in a typical surgical shift13.
Even though it was not measured in this study, micronutrients deficit such as iron, zinc, calcium, iodine, copper, selenium, vitamin E, and folic acid has also been described in college students. From these, calcium is one of the most important nutrients during youth; it is underprovided in 53% of students and has serious repercussions on bone health leading to osteopenia and osteoporosis14.
Sleep deprivation decreases retention of information, information processing, and decreases learning motivation. It has been reported that medical students with sleep deprivation describe themselves as inattentive15. In our group, medical students slept an average of 43.43 minutes per shift.
To the best our knowledge, this is the first study in which a nutritional balance between calorie intake and energy expenditure, sleep hours and activity is presented during a 24-hour shift in medical students. This might also be an attention call to the development of wellness programs in medical students with long-work hours, reduced sleep, intense activity and poor nutrition. Our group at Tec of Monterrey, has been working in the diagnose of our students physical and mental health and has proposed programs and adequations to overcome these situations, such as implementing personal tutoring, more effective learning scenarios (which leads to less clinical hours needed), meal quality improvement, psychological support, wellness center, recreating activities and learning communities among others.
One of our study limitations is that students were responsible to send pictures of the food intake during their shift, and even though ethical behavior is one of our institutional values, instructions were very clear, and a compromise agreement was signed by each participant, we are aware that information might have been manipulated or missing. Another drawback from our study is the small sample, but we believe this novel study would serve as reference to further research.
We are also aware that the photographic method for assessment of dietary quality is currently the method used for calorie intake measurement. Due to the complexity of medical interns´ shifts we were not able to apply this method, so we calculated calorie intake by using pictures recollected by mobile devices and estimating calories according to the portions from “Sistema Nacional de Alimentos Equivalentes”16. Despite this, canned or wrapped food represented 80% of the ingested calories in our study.
Conclusions
There is an important caloric deficit in medical students during surgical 24-hour shifts, additionally sleep deprivation is an important concern that must be elucidated in further studies. Strategies must be implemented to improve the quality and quantity of food consumed by medical students during their surgery rotations.
References